Introduction
Low back pain is one of the main reasons Americans visit their doctor. For adults over forty, it ranks third as a cause for doctor visits, after heart disease and arthritis. Eighty percent of people will have low back pain at some point in their lives. And nearly everyone who has low back pain once will have it again. Very few people who feel pain in their low back have a serious medical problem. Ninety percent of people who experience low back pain for the first time get better in two to six weeks. Only rarely do people with low back pain develop chronic back problems. Your doctor will evaluate your condition to make sure that no serious problems exist. Certainly, in some cases the problem can be serious and require more aggressive treatment--even surgery.
A definite cause of the pain cannot be determined in a large portion of cases. The spine changes as we age. Like skin that can become dry and wrinkled with age, the spine may also show normal signs of aging. These are natural changes that happen with the passing of time. Some people may experience pain from these changes; others don't. Changes in the spine that happen over time are referred to as degeneration or degenerative disc disease. Degeneration can be thought of as wear and tear that occurs each day as we use our spine for normal activities. Low back pain does not mean that you are destined to become disabled.
Causes
Why do I have low back pain? There are many causes of low back pain. Doctors are not always able to pinpoint the source of a patient's pain. But your doctor will make every effort to ensure that your symptoms are not from a serious medical cause, such as cancer or a spinal infection. The vast majority of back problems are a result of wear and tear on the parts of the spine over many years. This process is called degeneration. Over time, the normal process of aging can result in degenerative changes in all parts of the spine. Injuries to the spine, such as a fracture or injury to the disc, can make the changes happen even faster. There is strong evidence that cigarette smoking also speeds up degeneration of the spine. Scientists have found links among family members, showing that genetics plays a role in how fast these changes occur.
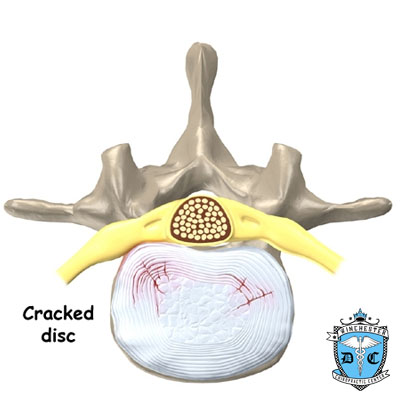
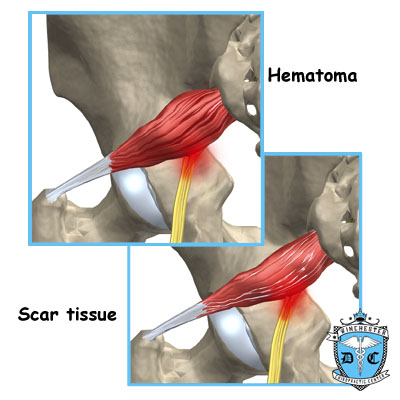
Degenerative Model The intervertebral disc changes over time. At first, the disc is spongy and firm. The nucleus pulposus portion in the center of the disc contains a great deal of water. This gives the disc its ability to absorb shock and protect the spine from heavy and repeated forces. The first change that occurs is that the annulus around the nucleus weakens and begins to develop small cracks and tears. The body tries to heal the cracks with scar tissue. But scar tissue is not as strong as the tissue it replaces. The torn annulus can be a source of pain for two reasons. First, there are pain sensors in the outer rim of the annulus. They signal a painful response when the tear reaches the outer edge of the annulus. Second, like injuries to other tissues in the body, a tear in the annulus can cause pain due to inflammation.
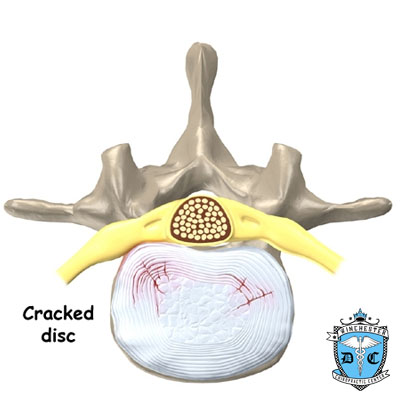
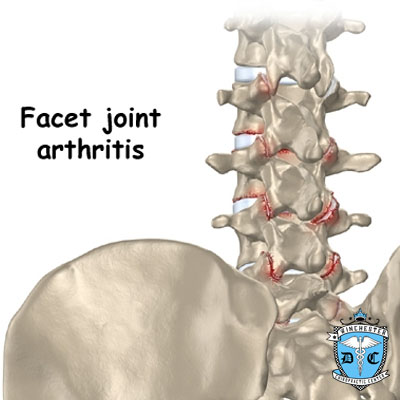
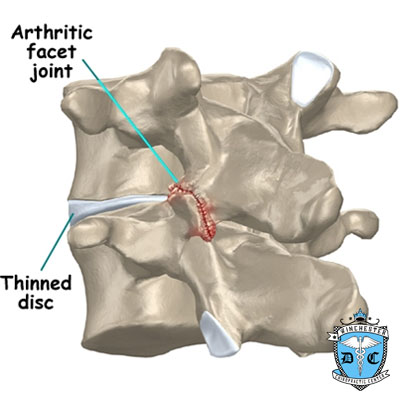
With time, the disc begins to lose water, causing it to lose some of its fullness and height. As a result, the vertebra begin to move closer together. As the disc continues to degenerate, the space between the vertebra shrinks. This compresses the facet joints along the back of the spinal column. As these joints are forced together, extra pressure builds on the articular cartilage on the surface of the facet joints. This extra pressure can damage the facet joints. Over time, this may lead to arthritis in the facet joints. These degenerative changes in the disc, facet joints, and ligaments cause the spinal segment to become loose and unstable. The extra movement causes even more wear and tear on the spine. As a result, more and larger tears occur in the annulus.
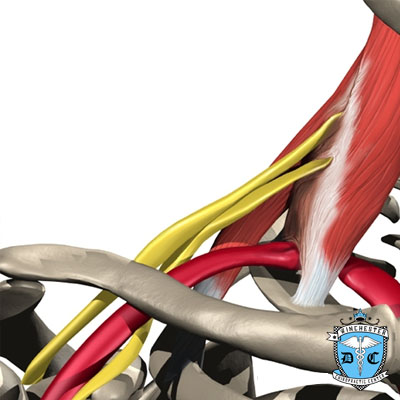
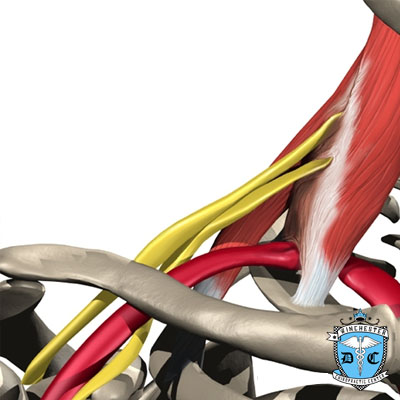
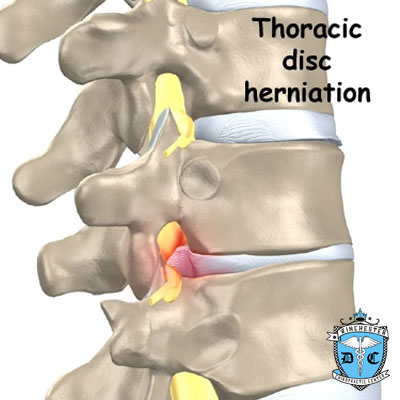
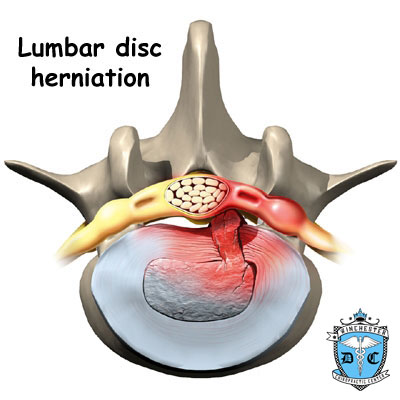
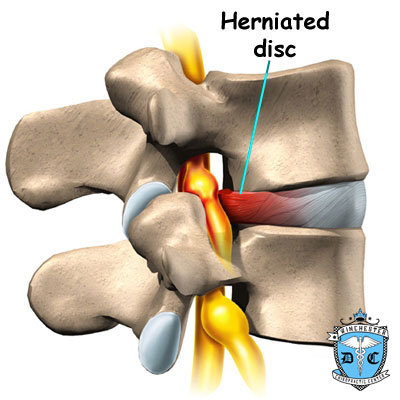
The nucleus may push through the torn annulus and into the spinal canal. This is called a herniated or ruptured disc. The disc material that squeezes out can press against the spinal nerves. The disc also emits enzymes and chemicals that produce inflammation. The combination of pressure on the nerves and inflammation caused by the chemicals released from the disc cause pain.
As the degeneration continues, bone spurs develop around the facet joints and around the disc. No one knows exactly why these bone spurs develop. Most doctors think that bone spurs are the body's attempt to stop the extra motion between the spinal segment. These bone spurs can cause problems by pressing on the nerves of the spine where they pass through the neural foramina. This pressure around the irritated nerve roots can cause pain, numbness, and weakness in the low back, buttocks, and lower limbs and feet.
A collapsed spinal segment eventually becomes stiff and immobile. Thickened ligaments and facet joints, scarred and dried disc tissue, and protruding bone spurs prevent normal movement. Typically, a stiff joint doesn't cause as much pain as one that slides around too much. So this stage of degeneration may actually lead to pain relief for some people.
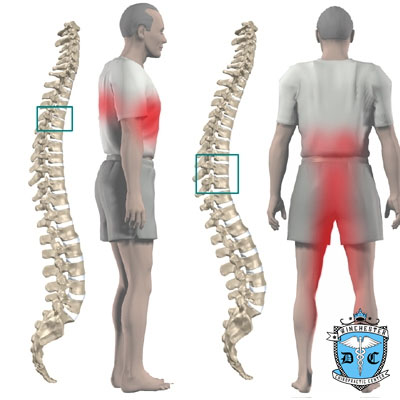
Mechanical Pain Mechanical back pain is caused by wear and tear in the parts of the lumbar spine. This type of pain is similar in nature to a machine that begins to wear out. Mechanical pain usually starts from degenerative changes in the disc. As the disc begins to collapse and the space between the vertebrae narrows, the facet joints may become inflamed. Mechanical pain typically gets worse after activity due to strain on the moving parts of the spine. Mechanical pain is usually felt in the back, but it may spread into the buttocks, hips, and thighs. The pain rarely goes down past the knee. Mechanical back pain usually doesn't cause weakness or numbness in the leg or foot, because the problem is not from pressure on the spinal nerves.
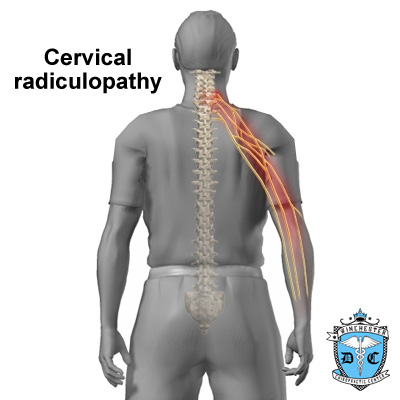
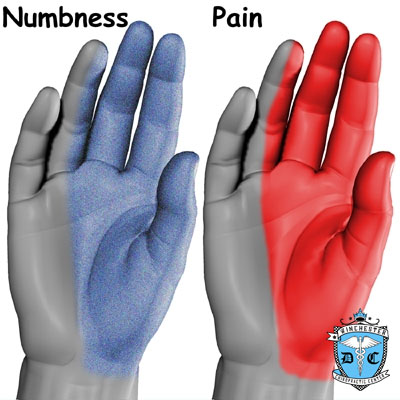
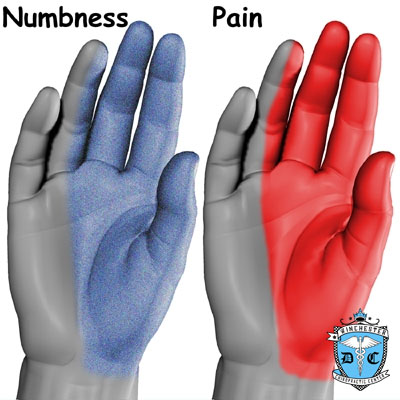
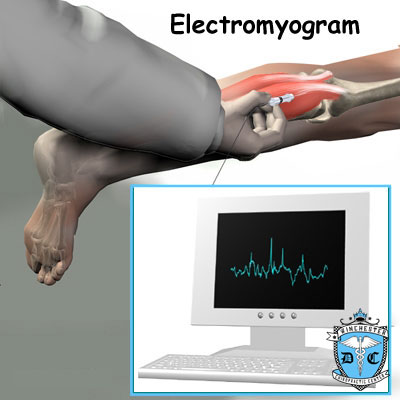
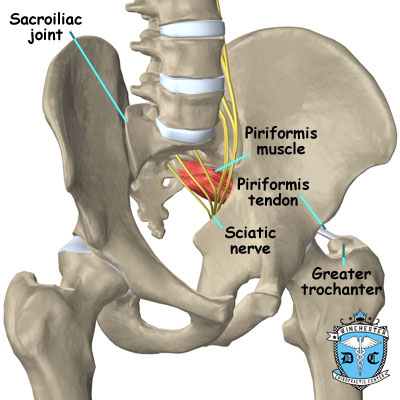
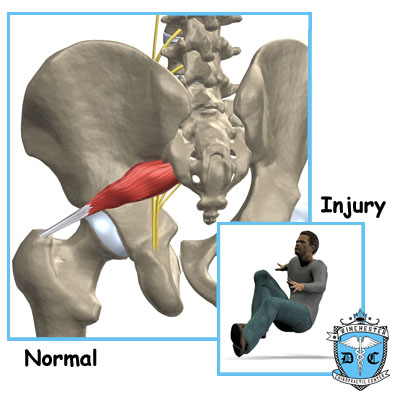
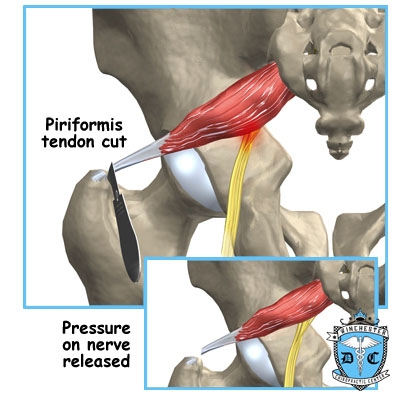
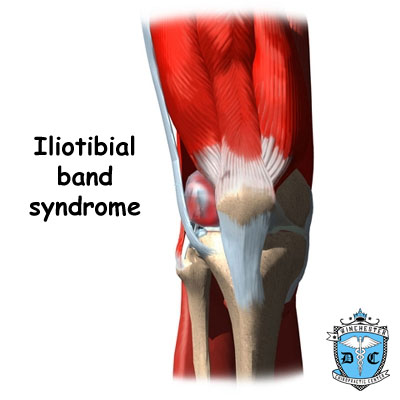
Neurogenic Pain Neurogenic pain means "pain from nerve injury." Neurogenic pain occurs when spinal nerves are inflamed, squeezed, or pinched. This can happen when a disc herniates or when a nerve gets pinched where it leaves the spine. Recently it has also become known that when a disc ruptures, chemicals are released that inflame the nerves even if there is no pressure directly on the nerve. Neurogenic symptoms concern doctors more than mechanical pain because it can damage the nerves and lead to weakness or numbness in the lower extremities. The nerve pressure causes symptoms in the areas where the nerve travels, rather than in the low back. This happens because pressure on the spinal nerve affects structures away from the spine, such as the muscles energized by the nerves. As a result, a person's back may not hurt, yet the person feels pain, numbness, or weakness in his or her leg or foot. This indicates there's a problem with the body's electrical wiring. The pressure on the nerve affects how the body functions. Muscles weaken. Reflexes slow. Sensations of pins, needles, and numbness may be felt where the nerve travels.
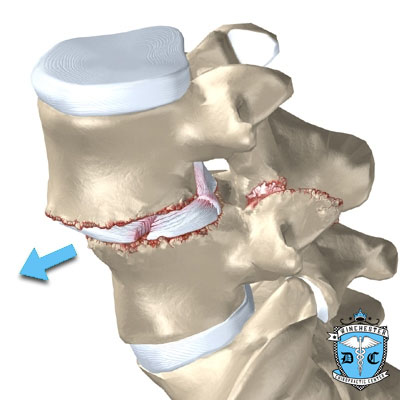
Annular Tears Our intervertebral discs change with age, much like our hair turns gray. Perhaps the earliest stage of degeneration occurs due to tears that occur in the annulus. These tears can result from wear and tear over a period of time. They can also be the result of a sudden injury to the disc due to a twist or increased strain on the disc that overpowers the strength of the annulus. These annular tears may cause pain in the back until they heal with scar tissue.
Internal Disc Disruption Multiple annular tears can lead to a disc that becomes weak. The disc starts to degenerate and collapse. The vertebrae begin to compress together. The collapsing disc can be the source of pain because it has lost the ability to be a shock absorber between the vertebrae. This condition is sometimes referred to as internal disc disruption. This type of problem causes primarily mechanical back pain due to inflammation of the disc and surrounding structures.
Herniated Disc A disc that has been weakened may rupture, or herniate. If the annulus ruptures, or tears, the material in the nucleus can squeeze out of the disc, or herniate. A disc herniation usually causes compressive problems if the disc presses against a spinal nerve. The chemicals released by the disc may also inflame the nerve root, causing pain in the area that the nerve root travels down the leg. This type of pain is referred to as sciatica. Even a normal disc can rupture. Heavy, repetitive bending, twisting, and lifting can place too much pressure on the disc, causing the annulus to tear and the nucleus to rupture into the spinal canal.
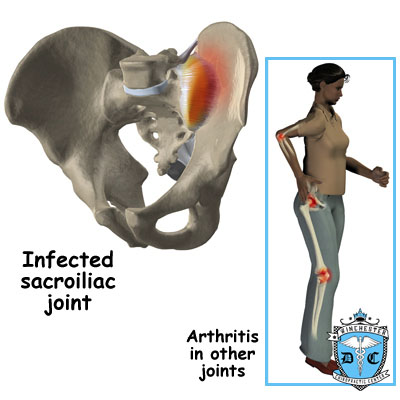
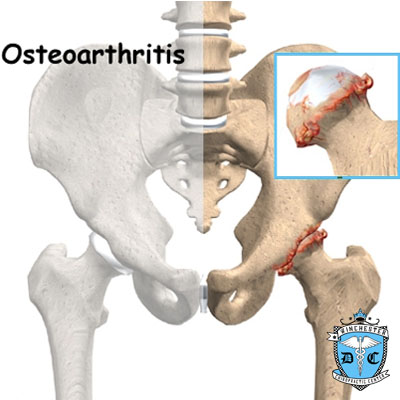
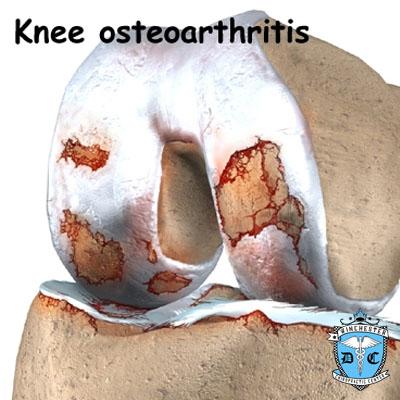
Facet Joint Arthritis The facet joints along the back of the spinal column link the vertebrae together. They are not meant to bear much weight. However, if a disc loses its height, the vertebra above the disc begins to compress toward the one below. This causes the facet joints to press together. Articular cartilage covers the surfaces where these joints meet. Like other joints in the body that are covered with articular cartilage, the facet joints can develop osteoarthritis as the articular cartilage wears away over time. Extra pressure on the facet joints, such as that from a collapsing disc, can speed the degeneration in the facet joints. The swelling and inflammation from an arthritic facet joint can be a source of low back pain.
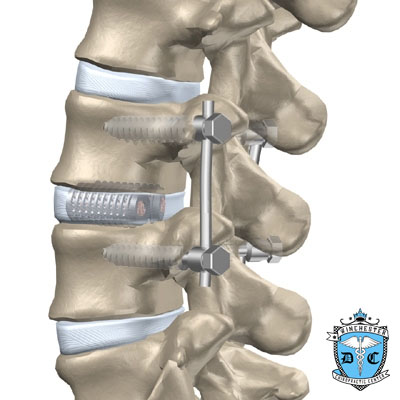
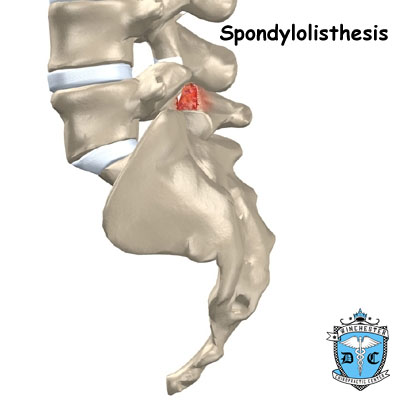
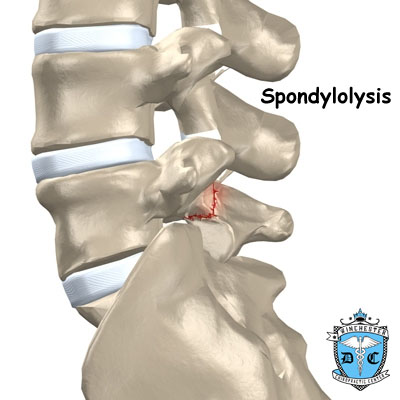
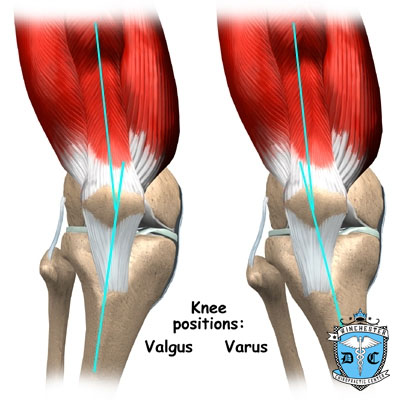
Segmental Instability Segmental instability also includes conditions in which a vertebral body begins to slip over the one below it. When a vertebral body slips too far forward, the condition is called spondylolisthesis. Whatever the cause, this extra movement in the bones of the spine can create problems. It can lead to mechanical pain simply because the structures of the spine move around too much and become inflamed and painful. The extra movement can also cause neurogenic symptoms if the spinal nerves are squeezed as a result of the segmental instability.
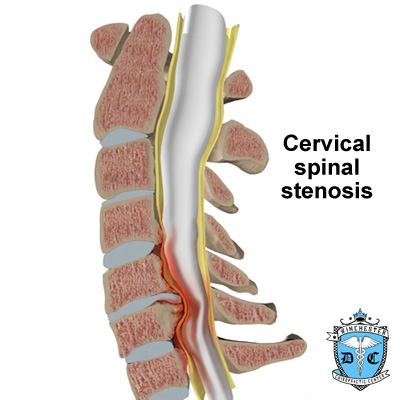
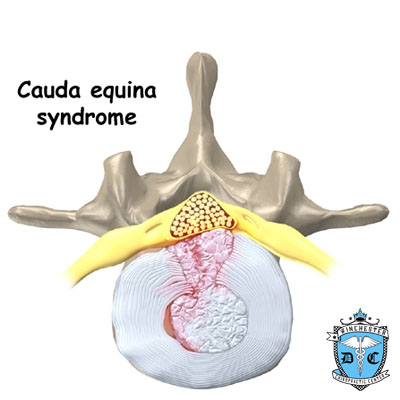
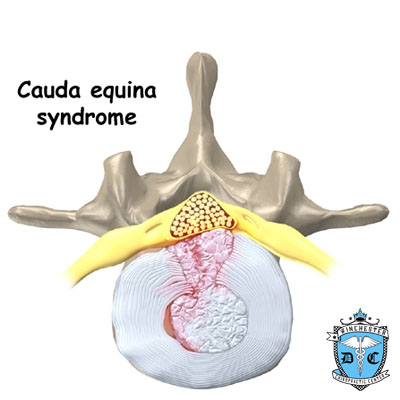
Spinal Stenosis Stenosis means "closing in." Spinal stenosis refers to a condition in which the tissues inside the spinal canal are "closed in," or compressed. The spinal cord ends at L2. Below this level, the spinal canal contains only spinal nerves that travel to the pelvis and legs. When stenosis narrows the spinal canal, the spinal nerves are squeezed inside the canal. The pressure from the condition can cause problems in the way the nerves work. The resulting problems include pain and numbness in the buttocks and legs and weakness in the muscles supplied by the nerves. Because these nerves travel to the bladder and rectum, weakness in the these muscles can cause problems with control of the bladder and bowels.
Foraminal Stenosis Spinal nerves exit the spinal canal between the vertebrae in a tunnel called the neural foramen. Any thing that causes this tunnel to become smaller can squeeze the spinal nerve where it passes through the tunnel. This condition is called foraminal stenosis, meaning the foramen is narrowed. As the disc collapses and looses height, the vertebral body above begins to collapse toward the one below. The opening around the nerve root narrows, squeezing the nerve. Arthritis of the facet joints causes bone spurs to form and point into the foramen, causing further nerve compression and irritation. Foraminal stenosis can cause a combination of mechanical pain and neurogenic pain from the irritated nerve root.
Symptoms
What are some of the symptoms of low back problems? Symptoms from back problems vary. They depend on a person's condition and which structures are affected. Some of the more common symptoms of low back problems are low back pain, pain spreading into the buttocks and thighs, pain radiating from the buttock to the foot, back stiffness and reduced range of motion, muscle weakness in the hip, thigh, leg, or foot, sensory changes (numbness, prickling, or tingling) in the leg, foot, or toes.
Rarely, symptoms involve changes in bowel or bladder function. A large disc herniation that pushes straight back into the spinal canal can put pressure on the nerves that go to the bowels and bladder. The pressure may cause symptoms of low back pain, pain running down the back of both legs, and numbness or tingling between the legs in the area you would contact if you were seated on a saddle. The pressure on the nerves can cause a loss of control in the bowels or bladder.
This is an emergency. If the pressure isn't relieved, it can lead to permanent paralysis of the bowels and bladder. This condition is called cauda equina syndrome. Doctors recommend immediate surgery to remove pressure from the nerves.
 Treatment
Treatment
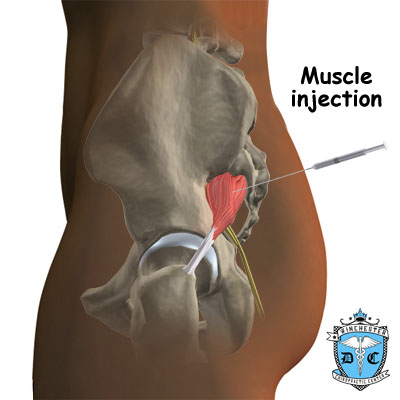
Low back pain is the number one reason patients seek care at the Winchester Hospital Chiropractic Center. We see hundreds of patients a week for this condition alone. Manual treatments such as spinal manipulation have been shown to be the most effective in treating people with lower back pain. Chiropractic doctors are the experts in spinal adjustments and manipulation. In fact, chiropractors perform 94% of all spinal manipulations in the United States. The remaining 6% are made up of physical therapists, medical doctors and osteopathic doctors. The chiropractic doctors at Winchester Hospital are trained in the latest adjusting techniques. You will also be taught neutral spinal postures aimed at decreasing pain, improving mobility, strength and function. Patients are taught how to protect their spines and prevent the problems from returning again. Strengthening exercises are also incorporated. Treatments are often combined with electrical muscle stimulation, ice, ultrasound, exercises, exercise balls, soft tissue massage, and traction. All of these are designed to help decrease pain and inflammation and improve function and mobility. Please see treatment sections to read further about these procedures.
Aerobic exercises may include walking on a treadmill, riding a stationary bike, or swimming. These activities can relieve the stress of low back pain, and they can cause your body to release endorphins into the blood stream. Endorphins are the body's own natural painkillers. An active approach to treatment helps patients attain better muscle function, so they can get their activities done easier. Active chiropractic rehabilitation speeds recovery, reducing the possibility that back pain will become a chronic problem. Along with active exercise, this format is used to help patients resume normal activity as swiftly as possible. Though patients are cautioned about trying to do too much, too quickly, they are guided toward returning to their activities. Pain is used to gauge the upper limits of activity. This approach gives patients a greater sense of control. They take an active role in learning how to care for their back pain. Treatment sessions focus on reassuring patients that getting back to work and other normal activities swiftly won't cause harm and can actually help them get better faster.
When needed, patients are encouraged to take certain actions to improve their spine health. Patients who smoke are encouraged to get help to quit. Because of the limited blood supply in the tissues of the low back, smoking speeds the degenerative process and impairs healing. Patients who are out of shape are encouraged to get fit. This strategy makes it less likely that back pain or injury will strike again in the future.
Dr. Kane and Dr. Zohn will show you how to keep your spine safe during routine activities. You'll learn about healthy posture and how posture relates to the future health of your spine. And you'll learn about body mechanics, how the body moves and functions during activity. Chiropractors teach safe body mechanics to help you protect the low back as you go about your day. This includes the use of safe positions and movements while lifting and carrying, standing and walking, and performing work duties. If indicated, your chiropractic doctor will work closely with your medical doctor and employer to help you get back on the job as quickly as reasonably possible. You may be required to do lighter duties at first, but as soon as you are able, you'll begin doing your normal work activities. Your chiropractor can do a work assessment to make sure you'll be safe to do your job. Dr. Kane and Dr. Zohn may suggest changes that could help you work safely, with less chance of re-injuring your back.
If you are concerned about your back, please do not hesitate to call us
781-933-5051 so that we can determine if it's time to visit our
practice.